
Quick Links
Resources
About MyLeukemiaTeam
Powered By





Leukemia is a type of blood cancer in which the bone marrow makes too many abnormal white blood cells, also known as leukocytes. As more cells are made, they begin to crowd out the body’s healthy blood cells, leading to leukemia symptoms. Monocytes are one type of white blood cell that is overproduced in leukemia.
High levels of monocytes or other white blood cells can give your doctor clues about which specific type of leukemia you have. Your monocyte count, along with other results from blood tests, may help your doctor determine which treatment regimen to recommend for your leukemia.

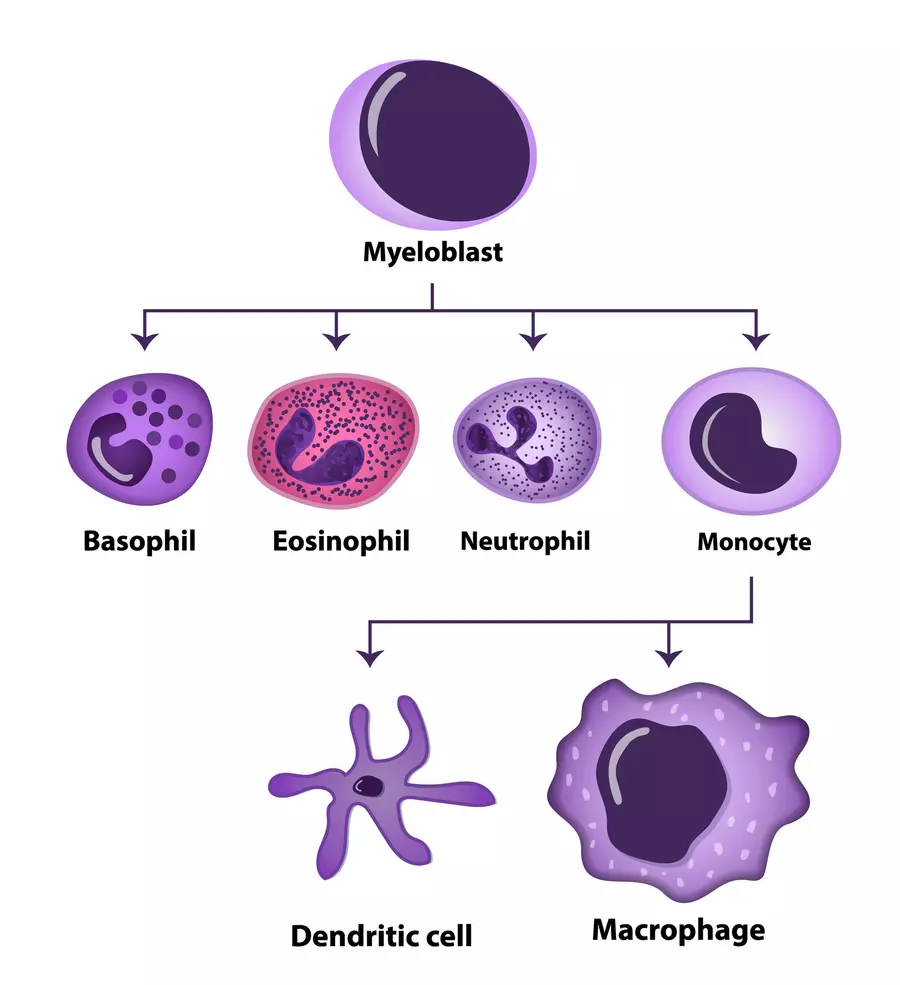
Monocytes are produced in the bone marrow but circulate widely in the blood. During an infection, the immune system activates monocytes to destroy invading germs. Other types of white blood cells include lymphocytes (T cells and B cells) and granulocytes (neutrophils, eosinophils, and basophils).
Monocytes usually circulate throughout the bloodstream, spleen, and bone marrow. To become activated, they must come into contact with inflammatory signaling molecules. When monocytes meet signaling molecules that indicate the presence of an infection, they mature into one of two types of innate effector (first-responding) immune cells — dendritic cells or macrophages. These are specialized cells known as antigen-presenting cells. Antigens are substances, usually foreign proteins such as viral or bacterial particles, that catch the attention of the immune system.
Dendritic cells travel to different areas of the body and pick up antigens. The dendritic cells then “present” these proteins to other immune cells, spreading the message of an infection or cancer and rallying an immune attack. Macrophages also present antigens to other immune cells but have other functions, too. For example, they surround and kill bacteria and infected cells and clear dead cells from the body.
Blood cell counts are measured using a test known as a complete blood count (CBC). This blood test measures your levels of white blood cells, red blood cells, and platelets to help your doctor get a complete look at your health. The counts are measured in cells per microliter of blood. An absolute monocyte count, which multiplies the CBC’s percentage of monocytes by the total number of white blood cells, may also be performed.
Normally, monocytes account for 2 percent to 8 percent of cells circulating in the blood, or 200 to 800 cells per microliter of blood. Levels that are lower or higher than normal may point to an underlying health condition. An abnormally high monocyte level is known as monocytosis and may be a sign of cancer, an autoimmune disease, or a mononucleosis infection. An abnormally low monocyte count, or monocytopenia, may be caused by aplastic anemia (low red blood cell count), a bacterial infection in the blood, or chemotherapy.

Monocyte counts vary among people but should generally fall within the normal range. However, high counts occur in certain types of cancer, especially chronic and acute myelomonocytic leukemia and acute monocytic leukemia. In these conditions, monocytes are not normal and don’t function effectively in their usual role. Treatments focus mainly on reducing the numbers of white blood cells and immature monocytes, which are known as myeloblasts or simply blasts.
Chronic myelomonocytic leukemia (CMML) is characterized by high levels of blasts that can’t function properly. Eventually, these immature cells crowd out healthy, mature cells and cause CMML symptoms.
Even though the condition has “leukemia” in its name, CMML is classified as a myelodysplastic syndrome/myeloproliferative neoplasm because of abnormalities in monocyte count and red blood cell production. Sometimes, CMML progresses and turns into acute myeloid leukemia (AML).
Monocyte levels for those with CMML are at least 1,000 per microliter of blood. Excess monocytes also build up in the bone marrow and interfere with the normal production of other types of blood cells, such as red blood cells and platelets. Low red blood cell counts prevent oxygen from reaching the body’s tissues, which leads to anemia and symptoms of fatigue, pale skin, and chest pain. Thrombocytopenia (low platelet count) may cause you to bleed and bruise easily. Monocytes may also build up in body organs, leading to symptoms such as an enlarged spleen.
The possible cure for CMML involves chemotherapy followed by a bone marrow transplant. For cases in which transplant isn’t possible, CMML can be managed with chemotherapy to help lower white blood cell counts.
Elevated monocyte levels in AML may be diagnosed as a specific subtype. These guidelines, which follow the French-American-British classification of AML, are based on how leukemia cells look under a microscope and on elevated levels of different immune cells.
Acute myelomonocytic leukemia (AMML, or AML-M4) is diagnosed based on higher monocyte and neutrophil levels. In AMML, blasts make up more than 20 percent of the blood and bone marrow. Additionally, mature monocytes and neutrophils make up at least 20 percent of bone marrow cells. Between 5 percent and 10 percent of AML cases are AMML, according to Leukaemia Care. Like CMML, the condition can also cause anemia and thrombocytopenia.
Treatments for AMML aim to reduce blast levels to below 5 percent and bring blood counts to normal ranges. Ideally, treatment includes induction chemotherapy to kill as many blasts as possible in the bone marrow and blood to achieve remission (reduced signs and symptoms of cancer). This can be followed with an allogeneic bone marrow transplant, which uses cells from a healthy donor.
Acute monocytic leukemia (AML-M5) — also known as acute monoblastic leukemia — is a common AML subtype that is diagnosed when 80 percent of leukemia cells come from monocytes or promonocytes (precursor cells to monocytes). It can be divided into two groups — AML-M5a and AML-M5b — depending on the types of monocytes found in the blood and bone marrow. AML-M5 is treated with induction chemotherapy and bone marrow transplant.
MyLeukemiaTeam is the social network for people with leukemia and their loved ones. On MyLeukemiaTeam, more than 12,000 members come together to ask questions, give advice, and share their stories with others who understand life with leukemia.
Have your blood test results shown high monocyte counts? Do you still have questions about what those results might mean for your leukemia? Share your experiences in the comments below, or start a conversation by posting on your Activities page.
Get updates directly to your inbox.



My Wife Has AML IDH1 & IDH2, Are They Treated With The Same Drug?
Sign up for free!
Become a member to get even more




A MyLeukemiaTeam Subscriber
I have CLL... This is good reading..
We'd love to hear from you! Please share your name and email to post and read comments.
You'll also get the latest articles directly to your inbox.